From basic physiology to clinical research
Brief Introduction
The Dyspnea Lab at Harvard (Headed by Bob Banzett and Bob Lansing) worked for more than 3 decades to discover the basic neural mechanisms underlying the symptom of dyspnea (shortness of breath, breathlessness). We utilized methods from respiratory physiology, experimental psychology, and neuroscience. Using pharmacological interventions, clinical lesions, and functional brain imaging we defined neural pathways and brain regions subserving dyspnea. We went on to improve measurement of dyspnea, and to apply what we had learned to clinical investigation.
(Disclaimer - this website emphasizes the significant contributions of the Dyspnea Lab, but we could not have done so much without the terrific work of the many scientists who went before us and beside us. They are generally not cited on this website, but they are cited in our published papers.)
Lab closed, education goes on
March 2024: Although the lab is closed now, we are rebuilding this website to include summaries of our work, links to our papers, and educational videos. This site will continue to grow throughout the year. Please check back later. Our comprehensive review of Air Hunger is now available in free PMC form. CLICK HERE
Upcoming event
Join us for Dyspnea 2026 in Lund, Sweden! This is a 2 1/2 – day international scientific meeting for physiologists, psychologists, neuroscientists, and clinicians with an interest in dyspnea research. Visit https://dyspneasociety.org/index.html for more info.
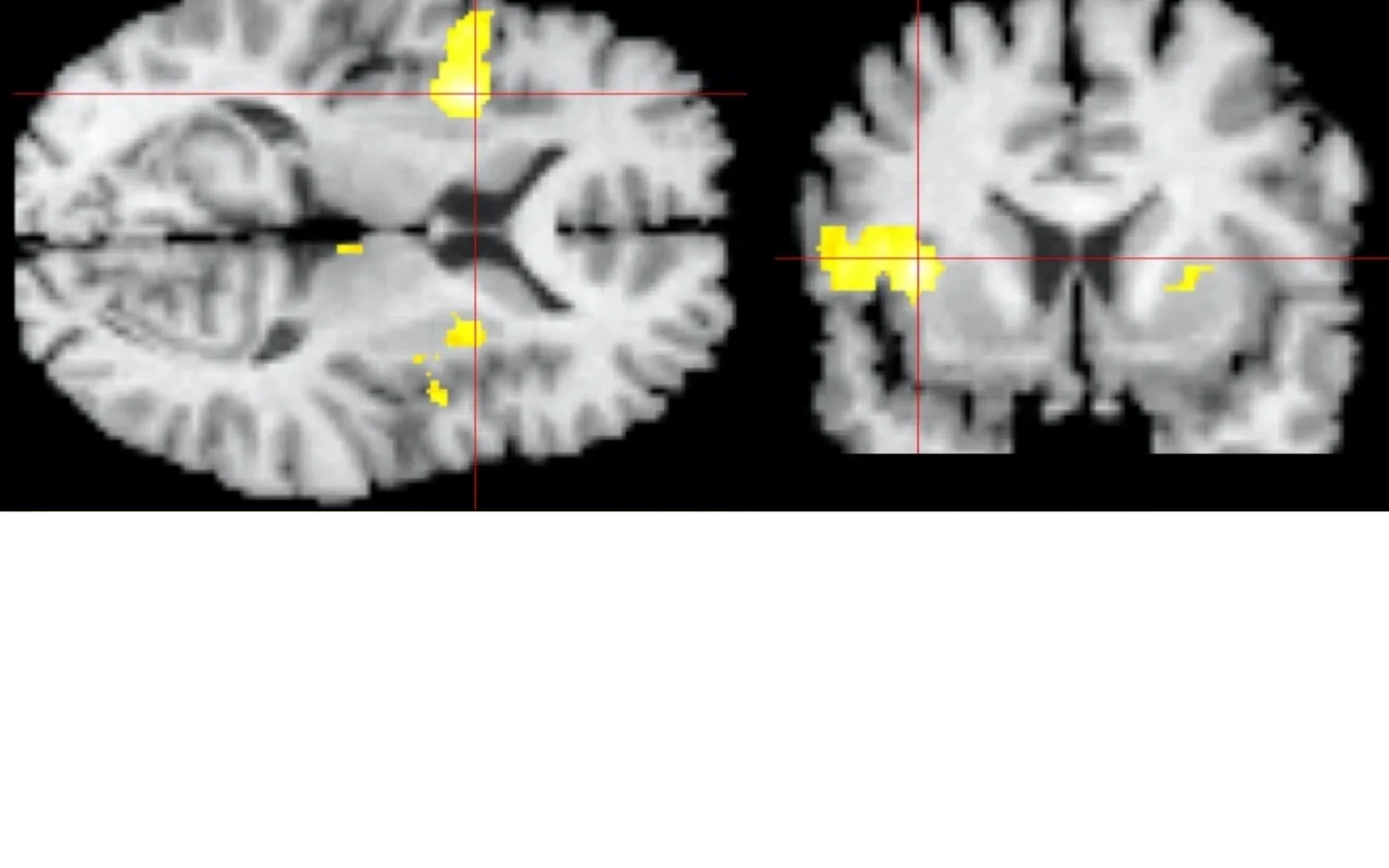
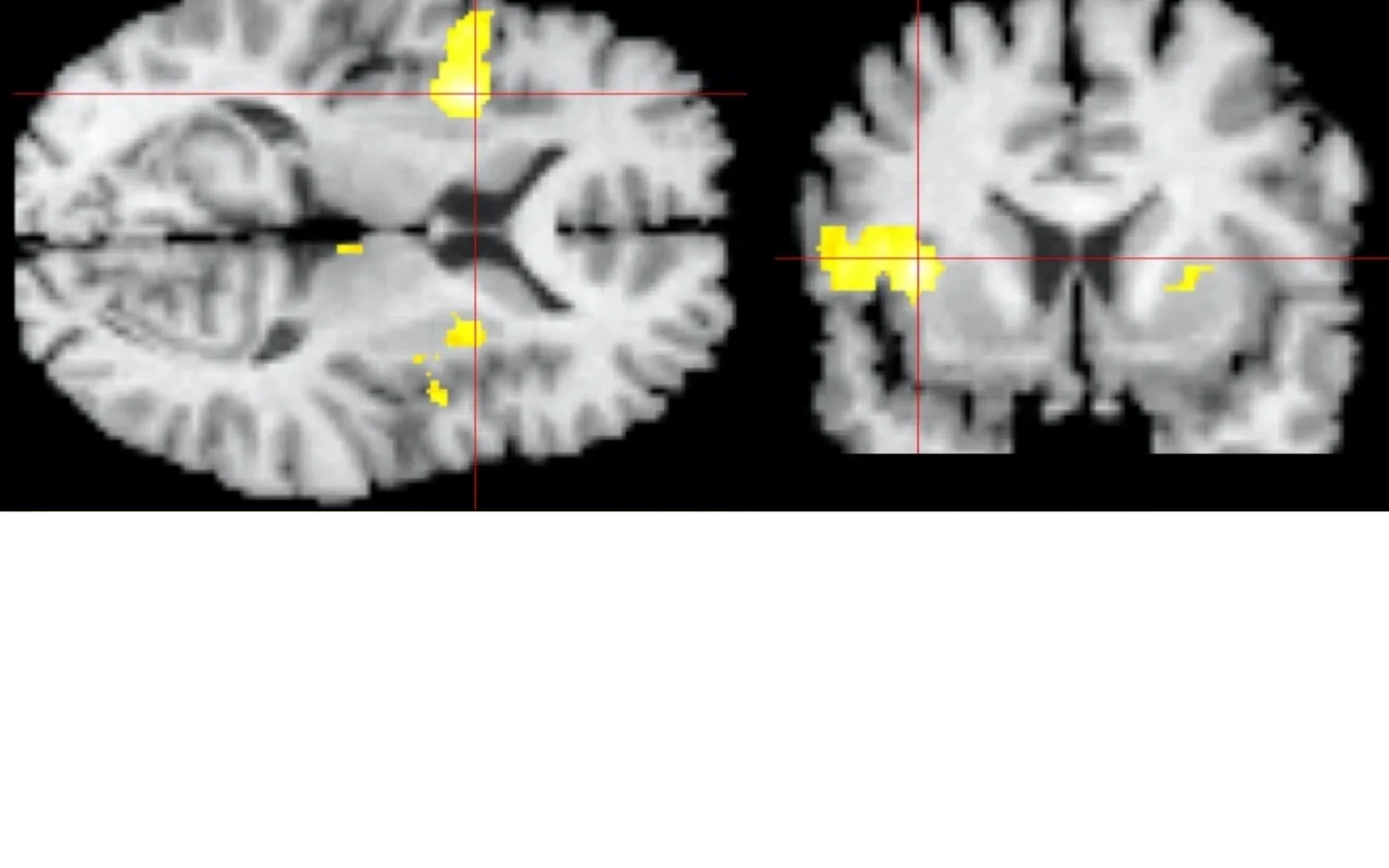
What is that image at the top of the page?
The image shown in the header is the first functional brain image of dyspnea. Dyspnea is a perceived sensation, thus it must be sited somewhere in the cerebral cortex. Prior to this image we had no idea where in the cortex dyspnea is perceived. The main activation found was in the right anterior insula, a location also important to perception of pain, thirst, and hunger.
(Banzett, Adams et al Neuroreport 2000)
Our research accomplishments

Neural Pathways
Dyspnea in the Cerebral Cortex
Dyspnea in the Cerebral Cortex
We developed laboratory models of dyspnea sensations. Using these models together with clinical and pharmacological neural lesions we identified peripheral and central neural pathways involved in dyspnea perception

Dyspnea in the Cerebral Cortex
Dyspnea in the Cerebral Cortex
Dyspnea in the Cerebral Cortex
Because dyspnea is consciously perceived, we knew it must be represented in the cerebral cortex, but, in contrast to other sensations such as touch, hearing, sight, pain, nobody knew what region of the cortex perceives dyspnea. We used functional brain imaging to discover the cortical sites involved in dyspnea perception.

Theory and Measurement
Dyspnea in the Cerebral Cortex
Theory and Measurement
We developed a theoretical framework in which dyspnea comprises several sensations. having a sensory quality and an affective component. Based on this, we developed a unified measurement instrument , the Multidimensional Dyspnea Profile (MDP).

Clinical translation
Dyspnea in the Cerebral Cortex
Theory and Measurement
We worked with nurses throughout our hospital to measure dyspnea in all patients. In addition to its value in symptom management, we found that patient-reported dyspnea strongly predicts adverse outcomes. We also used our laboratory models to examine effectiveness of interventions to relieve dyspnea.
Copyright © 2024 Dyspnea Lab - All Rights Reserved.
Powered by GoDaddy
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.